Changing of the guard: where AI x health priorities sit in summer 2024
Issue 82 l Eka’s Weekly Roundup (19 July 2024)
The UK’s impact scene doesn’t seem to be seeing any summer lull.
This week, we hosted & attended three catalytic events around Impact & Health, ranging from VC’s involvement in driving inclusive growth across the regions, to renewed excitement for health x ai in the investor & founder ecosystem, to changing priorities from the new government.
It’s a lot to unpack, but this is what we’ve been up to:
Impact Investing Workshop. We travelled to Manchester to attend the Impact Investing Institute’s latest roundtable around what the role of PE and VC should be in driving inclusive growth across the UK.
Health x AI community. We hosted 80+ innovators, investors, and CVCs in our offices during a (warm!) evening on Wednesday evening. It’s the second year we’ve been running this event and we’re thrilled to see the enthusiasm and excitement in the community.
AI in the NHS. The Health Foundation hosted a presentation on AI in NHS off the back of their Priorities for an AI in Health Strategy (thank you to Sergio from GSTT for flagging this to us!). We’ll explore this in more detail below.
The common thread across these events was excitement for innovation in the UK’s impact sector across diverse health vectors from prevention, to diagnostics, to treatment, and finally workflows.



Three (anti)-themes for AI in the NHS 🗞️
It’s important to remember that, not so long ago, (2018 to be precise), there had been discussions about whether the NHS should even be saved and remain a national institution. As an example, this chart from the Health Foundation which showed how health funding as a % of GDP had been slipping since 2009/10 until 2018/19 - not a great trend.
The picture today is more optimistic, though a lot of work will need to get done before we can be sure that the entire personal health journey is improved when considering 1) quality of life, 2) health equity, and 3) a “healthy” health workforce.
The Health Foundation’s event on Thursday discussed the potential of AI in healthcare, emphasizing the need for a robust evaluation framework, clear regulatory regime, and investment in healthcare workforce skills.
They also highlighted the importance of involving patients in AI development, scaling and industrializing AI use, and investing in people, particularly doctors. Speakers acknowledged the potential of technology to drive growth and sustainability in the National Health Service (NHS), but also raised concerns about prioritizing technology over sustainability and ensuring that the NHS remains equitable and responsible in its use of AI.
Let’s pick up on a few of these themes, in more detail.
Starting from the basics: fixing the foundations of the IT systems before thinking about a national-scale AI deployment strategy
As much as we talk about AI within the NHS, deployment is going to be a challenge if we still have non-systematised digital infrastructure across ICBs and more generally across the country.
(1) Digital infrastructure is a pre-condition for a lot of the exciting AI deployment.
A precondition to embracing AI is the modernization of NHS infrastructure across the stack. There is a risk that, by not getting the foundations right, we fall into the trap of “junk in junk out” and slowing down the old terminals even further.
Only then will the government be able to install a plan fore procurement give innovators a clear route to get their products into the NHS and into the places where they can make the greatest difference to patients. Karin Smyth MP here spoke about their planned NHS Innovation and Adoption Strategy (exact details still TBD).
(2) Our per-capita funding means that we can’t always invest in the foundational IT systems within the NHS
Funding models tend to be skewed to be on a per capita basis. Beneath this, we haven’t recognised the foundational investment as required in many of our institutions in the digital age.
Typically, the NHS will procure a software digital infrastructure data center, and then after you invest in x and x is the same for every institution, then you scaled up by how many people are actually served.
Because we have a legacy model of finding hospitals by the number of people for surveying, the challenges are that they can't afford the right digital infrastructure, the research and sustained investment and the people and the tools and technologies.
(3) It’s a people problem. Investing in the right AI talent and AI literacy is the other foundational layer we need to get right before accelerating AI deployment.
Haris Schuaib spoke about the People Problem. We can't have digital and data investment without investing in digital and data people. Similarly, we need need regulatory people who then operate that regulatory framework.
As Karin mentioned, cracking down on the NHS’s efficiency waste will help unlock savings to reinvest in people and technology which ultimately will help with AI literacy, cut waiting lists of patients, and ultimately improve patient care.
Move over doc, it’s the AI’s turn: how the dyadic relationship between doctor and patient could change to doctor, patient, and AI
(1) What happens when the AI human gets it wrong? Exploring duty of candour in this paradigm shift.
Let’s start off with a case study.
One speaker shared their lived example of an issue at St. Thomas’s hospital around pediatric bone need analysis. This is a process where you take an x ray of a young child’s hand and a radiologist pages through a book and ascribed a bone age to that child to see how well they're developing.
The clinicians had an incident where some of the consultant radiologists were complaining that the AI was getting it wrong. The AI deployment team had evaluated the program and it seemed to work fine.
The team investigated the problem and found that the AI was actually correctly doing the assessment. When children under the age of 4 come in and present a fracture, clinicians use the carpal bones to make this assessment. The AI was correctly doing it this part of the assessment. It turns out that the group of consultants were incorrect in their assessment.
(2) Communicating errors becomes very challenging in an era of dispersed responsibility and decision making.
In the example, who would bear the responsibility of telling the patient?
This specific scenario wasn’t that clinically serious. If it had been an oncology MDT where the AI and clinician had differing points of view, this would have been much more complex. How could this impact the clinician’s duty of candour? Is the dyadic relationship between doctor and patient now triadic?
There are no clear answers to these questions today, but the health system and its regulators will need to seriously consider the implications of AI decision making in the human context.
(3) There will always be tradeoffs in any AI deployment decision.
Changing systems will inevitably mean some tradeoffs. Rachel Power from the Patients Association laid these out clearly as:
AI efficiency vs human contact. AI efficiency may mean that there is less human contact over time (we only need to look at virtual GP appointments as an example of digital care here). However we would disagree with this tradeoff as, over time, we believe that the redistribution of clinicians time from administrative tasks to patient facing will be a positive one both for patients and clinicians wellbeing.
Rapid diagnostics vs explainability. Diagnostics can now happen at the first appointment - one example came up throughout the panel that there are some oncology disciplines which, in certain hospitals, can come up with a conclusive answer with a fast MRI test. This changes pathways as before, the patient would have gone home and waited before getting their diagnosis either face to face or through a letter depending on their choice. Over time we believe that systems will move towards high standards of explainability such that patients will get the benefits of fast turnaround diagnostics with high trust and fidelity in the clinicians and AI systems.
Personalisation vs standardisation. AI ushers in a new wave of personalisation within standards of care. But there are also some benefits to standardisation including the standards themselves. In a steady state we believe that we will find a point of balance across the two extremes with clear definitions for what requires standardisation and what adds more social value by being personalised.
What about prevention? Policy makers are focussing on the NHS itself, but omitted a prevention strategy for what sits before the health system.
(1) Policy is still early in setting out a detailed prevention and social care strategy.
The talk didn’t mention prevention or social care in any detail, which we thought was a slight change on Wes Streeting’s speech last week.
(2) There are four buckets of health which could be improved using AI from public health to workflows.
The Health Foundation did lay out the key application layers for AI within the health system.
Discovery across drug development, therapeutics, and medtech
Treatment diagnostics,
End-to-end pathways across primary, secondary, and community care,
Population health.
Today, the NHS and UK system has focussed largely on the first two buckets. However going forward, in order to lead to system change, we will need to address (3) and (4). There are some early green shoots, for example the NHS deploying AI to help target waiting lists and missed appointments.
We’re proud at Eka to support players across these verticals including Flok which is an end-to-end digital pathway for musculoskeletal disease, Isla which is the software provider for remote care delivery, and Oxcan which is a very early-stage lung cancer diagnostic which could over time prevent the most invasive treatments.
Week in Impact Articles ✍🏽
Monday: Consumer Trends 2024: Mid-Year Report
Wednesday: Progress on buildings circularity depends on 4 key elements
Thursday: The Key to Longevity is Boring
Friday: Heat waves: Why a hotter world might be a more dangerous, violent, and less productive one
3 Key Charts 📊
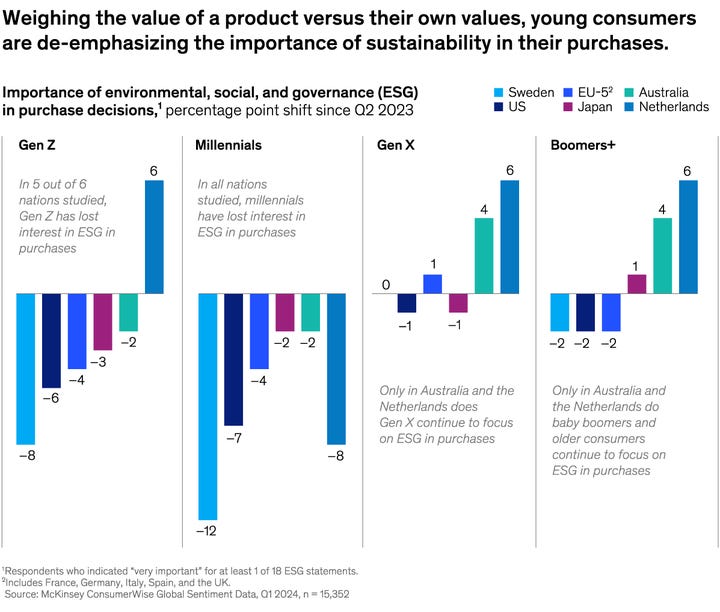
1. Changing tide? Gen-Z consumers directionally are weighing ESG considerations less.
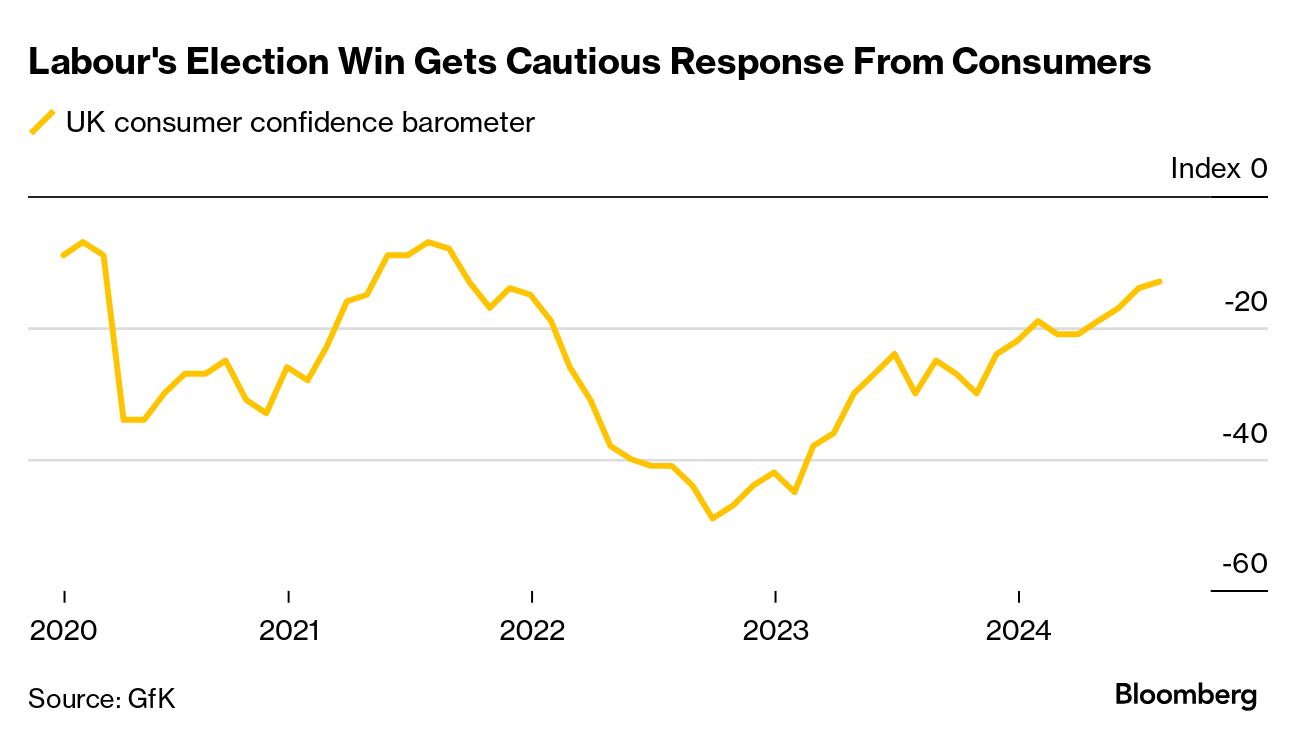
2. The UK’s consumer confidence on the rise, but still in negative territory
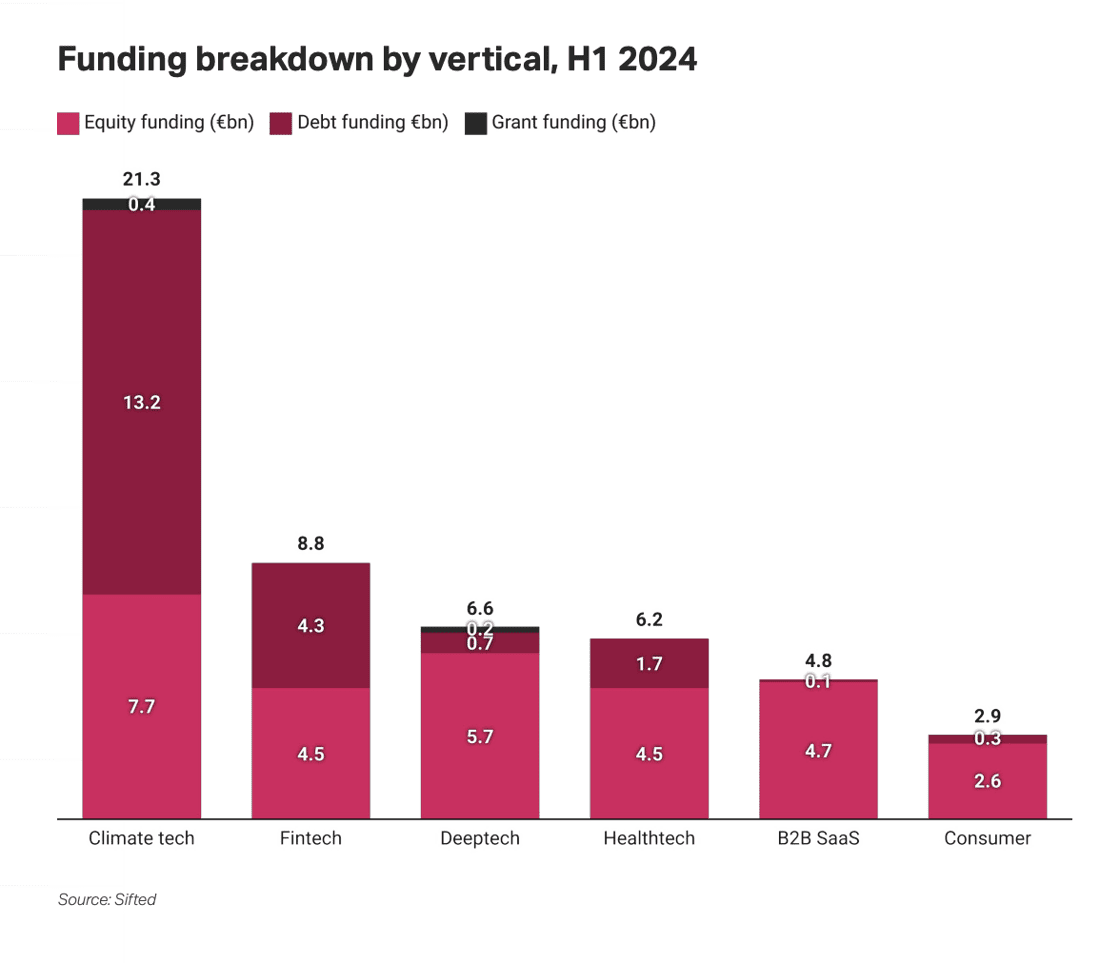
3. Debt in the stack: its increasing role within climate-tech
Getting in Touch 👋.
If you’re looking for funding, you can get in touch here.
Don’t be shy, get in touch on LinkedIn or on our Website 🎉.
We are open to feedback: let us know what more you’d like to hear about 💪.